Motor vehicle accidents can result in various severe injuries. When severe physical trauma occurs, there is often a long recovery period. In unfortunate instances, injuries or paralysis can be permanent.
Rehabilitation is often long, yet getting the proper treatment and care is as important as having emotional support.
Some of the most common injuries in severe motor accidents include:
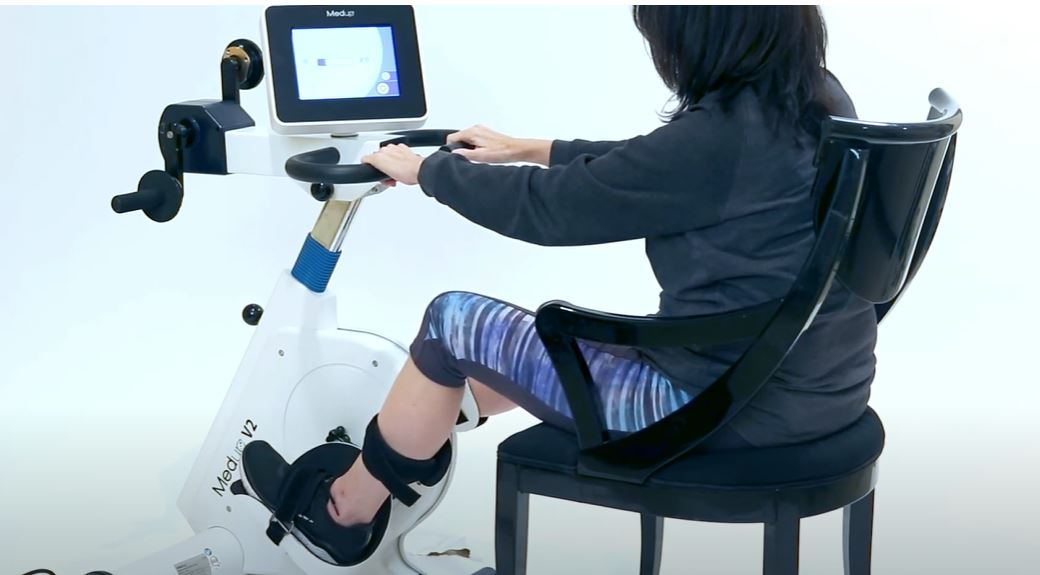
The MedupV2 is an advanced, therapeutic cycle trainer that can be at the centre of a post-accident rehabilitation program. Exclusively available in Ontario here and available to institutions and individuals. Contact us.
- Traumatic Brain Injury (TBI): A TBI occurs when a sudden impact or jolt to the head disrupts normal brain function. It can range from mild concussions to more severe injuries with long-lasting effects on cognitive abilities, motor skills, and emotional well-being.
- Spinal Cord Injuries: These injuries can lead to partial or complete paralysis, depending on the severity and location of the damage. Spinal cord injuries often result in significant physical impairments and may require long-term rehabilitation and adaptive strategies for daily living.
- Fractures and Bone Injuries: High-impact collisions can cause fractures in various bones, such as the arms, legs, ribs, and pelvis. These injuries may necessitate surgeries, immobilization through casts or braces, and extensive rehabilitation to regain strength and mobility.
- Internal Organ Damage: The force involved in a motor vehicle accident can cause internal injuries to organs like the liver, spleen, kidneys, or lungs. These injuries may require surgical intervention and close monitoring to prevent complications.
- Limb Amputations: Severe accidents can result in traumatic amputations, where a limb is partially or entirely severed during the collision. Amputations have profound physical and psychological impacts, and individuals may need specialized prosthetic limbs and extensive rehabilitation to adapt to their new circumstances.
- Facial Injuries: High-speed collisions can lead to facial trauma, including fractures of the jaw, cheekbones, or nose. Facial injuries may require reconstructive surgeries and specialized treatments to restore function and aesthetics.
- Whiplash and Neck Injuries: Whiplash occurs when the head is forcefully jerked forward and backward, causing soft tissue damage in the neck. This can result in pain, stiffness, and reduced range of motion, requiring physical therapy and pain management techniques.
These injuries can have long-lasting consequences and may require comprehensive medical care, rehabilitation, and psychological support. In all cases, prompt diagnosis and care should precede a comprehensive recovery plan.
Active Passive Cycle Training Supports Motor Vehicle Recovery
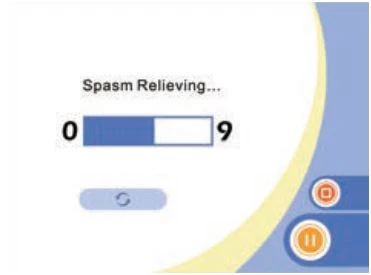
An active passive cycle trainer can potentially help with recovery after a severe motor accident. An active passive cycle trainer, also known as a motorized or electrically assisted cycle, is a rehabilitation device that combines both active and passive cycling. It allows the user to actively pedal the bike while also providing assistance when needed.
Key benefits of active-passive cycling
- Muscle Activation: The active pedaling motion on the cycle trainer helps to activate and strengthen the muscles involved in cycling, such as the quadriceps, hamstrings, and calf muscles. This can be beneficial for reconditioning the lower limb muscles and improving their strength and endurance.
- Joint Mobility: Regular cycling motion on the trainer can promote joint mobility and flexibility. It can help to prevent stiffness and improve range of motion in the hips, knees, and ankles, which may be affected after a motor accident.
- Cardiovascular Conditioning: Using the active passive cycle trainer can provide cardiovascular exercise and improve cardiovascular fitness. This can be especially important for individuals who have been immobilized or had reduced physical activity due to the motor accident.
- Neuromuscular Rehabilitation: Cycling on the trainer can assist in retraining and reconnecting the neural pathways between the brain and the lower limbs. This can be particularly beneficial for individuals who have experienced nerve damage or loss of motor control due to the accident.
- Psychological Well-being: Engaging in regular exercise, even in a rehabilitation setting, can have positive psychological benefits. It can help improve mood, reduce stress, and enhance overall well-being during the recovery process.
On the Road to Recovery and Restoring Motor Function
Importantly, the use of an active passive cycle trainer should be done under the guidance of a qualified healthcare professional or physical therapist.
Learning proper use of any advanced rehab cycle trainer is paramount, as much as the program for rehabilitation/exercise undertaken. Whether used within a hospital or institutional setting – or at home – frequent re-assessments can relate progress and inform the ongoing rehabilitation programming. With goal setting a progress measurement, the cycle trainer can become a central aid to safely promote recovery.